- Who We Are
- Clinician Employment
- Publications
- Witness to Witness (W2W)
- Kugel & Zuroweste Health Justice Award
- Your Voice Matters: Photovoice Project
I Worked at the ER Treating COVID-19 Patients, Then My Daughter Got Sick: Frustrations and Unknowns by MCN's Laszlo Madaras
Thu, 06/25/2020 | by Laszlo Madaras

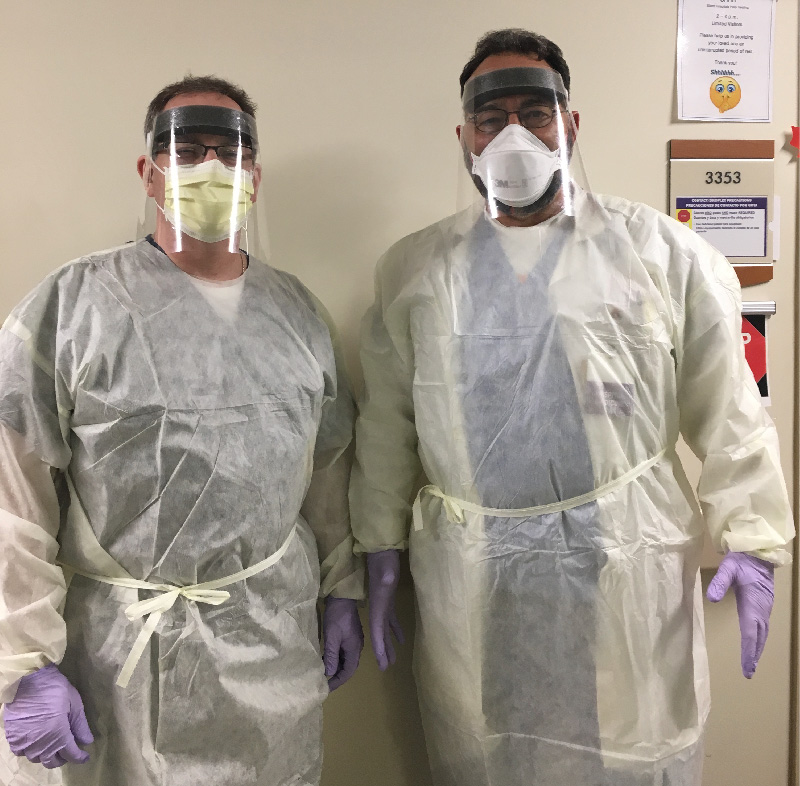
MCN's Dr. Laszlo Madaras (right) and a colleague wear PPE at their hospital in Pennsylvania.
By Laszlo Madaras, MD, MPH, Chief Medical Officer for the Migrant Clinicians Network
My daughter woke me up just after midnight in tears, telling me she suddenly awoke to a racing heartbeat and severe shortness of breath after going to bed just hours earlier and enjoying a deep sleep. She had me worried with a day of headaches followed by two days of fevers of 101 but no cough and, until now, no shortness of breath. We had decided to go to the COVID-19 tent set up outside of our hospital the following morning to get her checked for SARS-CoV-2, but this midnight episode precipitated a more urgent visit to the COVID-19 tent and to the emergency room itself.
I have worked in our 260-bed community hospital treating COVID-19 patients since this pandemic reached our region in the early spring of 2020. I was meticulous about not bringing the virus home, paying close attention to the series of WHO and CDC recommendations for use of personal protective equipment (PPE) as they evolved week by week. We are an easy day's drive from New York where we watched the pandemic blow up in that wonderful city which my daughter now calls home. She left the city around St. Patrick's day as a lockdown began and she wanted to return to rural Pennsylvania to quarantine with me. This gave me all the more reason to keep COVID-19 away from our doorstep. I showered, changed scrubs frequently, and left all masks and any hospital equipment either at work or in the car in a plastic bag. Never in the house. This plan worked for nearly four months, but this midnight episode of acute shortness of breath made me realize that, finally, I had failed to protect her. Together we drove to the hospital at a speed that I have not needed to use since I stopped delivering babies at that same hospital years ago. She became more tachypneic as she began to get anxious, and that increased her shortness of breath even more.
By the time we arrived at the hospital, her heart rate was over 140 and her fever again 101. My colleague, the ER doctor, took over and did all the usual tests including the nasopharyngeal swab for COVID-19. She did not have hypoxia (low oxygen saturation by pulse oximetry) but was tachypneic for another hour. This was the opposite of what I had found in many of my COVID-19 positive patients who were most often hypoxic but did not seem at first too bothered by it (the "happy hypoxics" as we originally called them). This is part of the mystery of learning every step along the way of this new disease, why we call it a novel virus. There are no rules, just observations over and over as we try to define what this virus can and cannot do.
By the end of the night she looked much better, no longer felt short of breath nor the need for oxygen, and ultimately she was discharged home in the morning. The nurse let us know that someone will call with the COVID-19 results but because she is not staying in the hospital, her results will not return as quickly as results for those patients who are being admitted.
The ER doctor was very thorough and ruled out pneumonia, pulmonary embolism, reactive airway disease. The only thing still pending was the COVID-19 testing, which in some cases comes back within four to six hours, often forty to sixty hours, and sometimes even longer. In our hospital, I saw a very slow return in March and early April; there were very few centers of testing and these labs were overwhelmed with the increasing demand. Then, in late April to mid-May (our busiest time), thankfully our region got more test sites and we were very fortunate to get a turnaround time of just a few hours of the nasopharyngeal swab. Then, late May to mid-June, when some of the reagents/chemicals needed for the testing were running out, we reverted back to a much slower testing turnaround time, which is where we were at this juncture as we left the emergency room. I thought to myself how hard it is to make consistent nationwide policy and recommendations when at just one institution there was this much internal variability. And my hospital is not unique in this way.
Ultimately, it took just over four days for the results to come back -- negative.
This brought up many more questions as well as frustrations about the unclear answers. How sure can we be that this was not a false negative when it seemed like everything else was ruled out? I have now had several dozen COVID-19 patients, and this was at the top of my differential diagnosis as most probable. Perhaps another spring virus? And it took so long to come back, does everyone have enough patience to self-quarantine and avoid contact while they wait? What does a negative mean here -- should she get retested or wait for the antibody testing later? These are questions I tackle with my hospital patients, and now it was something to deal with at home too.
Other frustrations of a long testing lag time include the needing to burn thru extra PPEs while slowly ruling out hospitalized patients for days and days in the hospital. Luckily, we have not seen much in-hospital patient-to-patient cross-infection as we have seen in other settings, like nursing facilities, meat packing plants, prisons, and military facilities. Still, it is concerning that the long delay in getting test results could theoretically lead to increased risk of a hospital-acquired COVID-19 infection. So I was glad that my daughter did not require hospitalization, although from then on I was a light sleeper at home, keeping the door open, hoping not to hear her struggling to breathe upstairs while she slept.
While we are grateful for the immediate, comprehensive, good care she received, we still have many frustrations with not knowing the testing specificity and sensitivity of various nasopharyngeal swabs; whether she would have tested positive had she tested a second time (I have seen this as a doctor); whether antibodies mean lifelong immunity or even temporary short term immunity; whether testing for antibodies with a blood test would be meaningless since she tested negative with the swab this one time; whether there is any longer term damage the virus could cause in years to come...
Less than 10 percent of Americans have been tested as of this writing, just after Father's Day 2020. As a father, as a doctor, as a neighbor who is now also the designated grocery shopper at the local stores while others quarantine, I share the frustration of many who would like truthful answers, better answers, more timely answers. I understand that we cannot be consistent one month to the next -- the data coming in is changing our view of this new virus on a weekly, often daily basis. That is how science works as new data come in, especially when we have not heard from over 90 percent of the Americans not tested. I also understand a frustrated public wanting more consistency in the recommendations based on the best science.
I have experienced this COVID-19 period in many ways -- first as a hospital doctor dealing with very sick patients, some of whom have died in the hospital alone; then as a professor trying to keep medical students from having direct contact with COVID-19 patients as required by their schools; also as a chief medical officer of an amazingly talented organization that is trying to give protective guidance to farmworkers and other essential workers most at risk for contracting COVID-19. And now finally as a father of someone who may or may not carry the virus, but certainly behaves in a frightening way very much like someone who was sick with SARS-CoV-2. My daughter has recovered, but many unknowns remain.
Like what you see? Amplify our collective voice with a contribution.
Got some good news to share? Contact us on our social media pages above.
Return to the main blog page or sign up for blog updates here.