- Who We Are
- Clinician Employment
- Publications
- Witness to Witness (W2W)
- El Premio Kugel & Zuroweste a la Justicia en la Salud
- Your Voice Matters: Photovoice Project

Diabetes is a leading chronic health condition among patients served by federally funded health centers, and the seventh leading cause of death in the US. Over 12 percent of Latino Americans suffer from diabetes, compared to 9.4 percent of the population overall.1 In addition to a greater prevalence, Latinos suffer worse outcomes. Latinos with diabetes are twice as likely to be admitted to a hospital for lower extremity amputations compared to non-Hispanic whites with diabetes, and are three times more likely to have end stage renal disease due to diabetes.2
Mi salud es me tesoro: una guia para vivir bien con diabetes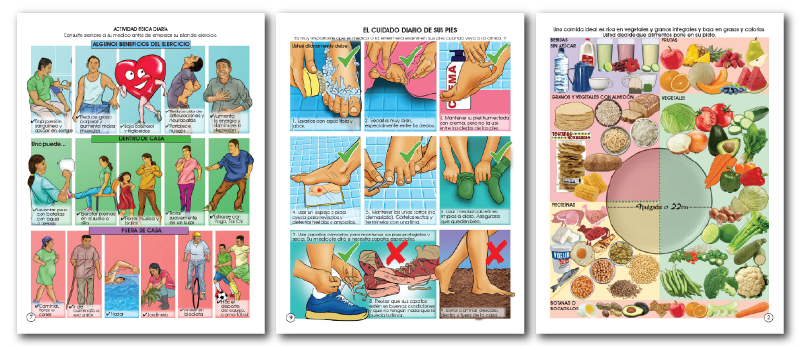
Diabetes is a common but complicated health condition facing agricultural workers within the United States. To help assist agricultural workers in learning about this diagnosis, Migrant Clinicians Network has partnered with professional artist and collaborator Salvador Sáenz to create “Mi salud es mi tesoro: Un guía para vivir bien con diabetes,” or, “My Health is My Treasure: A Guide to Living Well with Diabetes.” This Spanish-language, low-literacy comic book explores the topic through the full-color story of an agricultural farmworker named Goyo, whose recent diagnosis of diabetes prompts him to engage in conversations with other agricultural workers on topics of diet, exercise, and illness prevention while facing the unique hurdles of living a life of migration.
Download a digital copy of the comic book here
Among Migrants
While migrant-specific data are not widely available, this background on Latino Americans serves as a proxy; it is likely that migrants, the majority of whom would be classified as a subset of Latino Americans, experience even greater rates of disease complications due to occupational, socioeconomic, cultural and political factors. Some of these include:
- Cultural issues, such as language, literacy, medical knowledge, health care practices and beliefs, and dietary practices;
- Poverty, with unreliable transportation, lack of insurance and prescription coverage, inability to buy services and supplies or to modify diets, and substandard housing that may lack refrigeration, privacy, or adequate bath facilities;
- Migration, causing discontinuity of care and unfamiliar health care systems, as well as special needs related to traveling long distances;
- Political considerations associated with immigration status of the patient and family, and work environments that typically do not include benefits, supports and protections such as disability coverage or worker's compensation;
- Work environments that complicate the needs associated with foot care, glucose monitoring, hydration, rest, and self-medication.
“Juana*, a mobile agricultural worker with diabetes, has rarely left her agricultural worker housing in Upstate New York, because of her inflexible work schedule, her unfamiliarity with the community and her inability to speak English, and her anxiety around recent flare-ups of anti-immigration rhetoric in the community that other agricultural workers spoke about. With little education about her condition, she decided to ration her insulin rather than seek out a local clinic to refill her prescription. Without consistent medication, her diabetes may get out of control and she may end up in the emergency room.”
- Health Network case study

Improving Care, Improving Outcomes, and Reducing Cost
“Care for people with diagnosed diabetes accounts for 1 in 4 health care dollars in the U.S., and more than half of that expenditure is directly attributable to diabetes.” --American Diabetes Association
A substantial amount of US medical spending is spent serving patients with diabetes. Underserved patients like mobile workers often have trouble accessing care. Without well-patient diabetes visits, outreach programs, and diabetes self-management programs that take into account the limitations and disruptions that migration present, mobile patients may avoid care until health concerns are acute, more costly, and more difficult to treat. Several health center-focused initiatives have shown that proactive well-patient diabetes visits with an integrated care team fend off crisis management. Additionally, comprehensive care aided with culturally and linguistically appropriate group meetings led by Community Health Workers results in lower Hemoglobin A1c numbers.4 5
Resources
Migrant Clinicians Network provides health centers and other community health organizations with extensive technical assistance and training on diabetes. From our recent Project ECHO on diabetes and hypertension for Community Health Workers, to our webinar focused on diabetes and occupational health, MCN brings the latest data from the experts and the most effective diabetes care improvement models directly to the workers on the frontlines.
COMIC | Mi salud es me tesoro: una guia para vivir bien con diabetes
MCN’s Project ECHO page describes our recent Diabetes ECHO sessions, featuring leading diabetes experts engaging directly with Community Health Workers from around the country.
MCN's Diabetes Online Toolkit has a wealth of resources.
Health Network provides assistance for any patient on the move with an ongoing health concern, including diabetes.
MCN’s 2018 webinar, “The Impact of the Workplace on Primary Care Management of the Diabetic Patient,” establishes the many links between workplace and diabetes control.
Other resources:
Learning About Diabetes - Consumer Programs
References
1 American Diabetes Association. Statistics About Diabetes. http://www.diabetes.org/diabetes-basics/statistics/
2 Office of Minority Health. Diabetes and Hispanic Americans. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=63
3 American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2017. http://care.diabetesjournals.org/content/early/2018/03/20/dci18-0007
4 Gary TL, Bone LR, Hill MN, et al. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans. Prev Med. 2003;37(1):23–32.
5 Norris SL, Chowdhury FM, Van Le K, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;23(5):544–556.




