- Who We Are
- Clinician Employment
- Publications
- Witness to Witness (W2W)
- El Premio Kugel & Zuroweste a la Justicia en la Salud
- Your Voice Matters: Photovoice Project
Thu, 06/22/2017 | by Claire Hutkins Seda

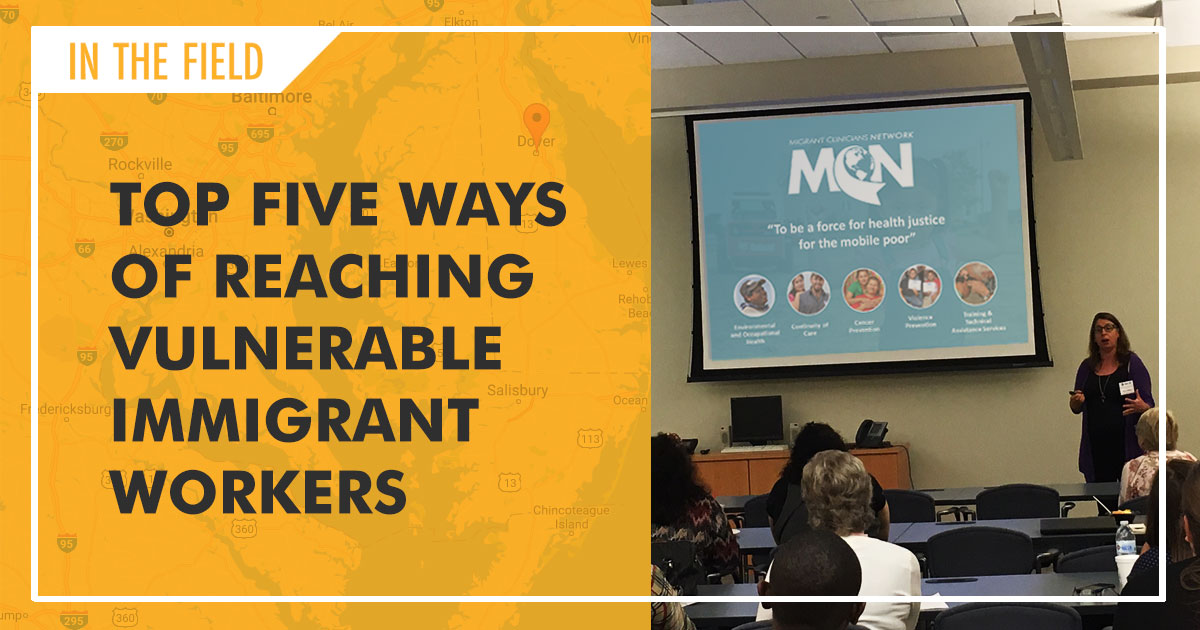
Earlier this week, Migrant Clinicians Network’s Amy K. Liebman, MPA, MA, Director of Environmental and Occupational Health, took a drive from MCN’s Maryland office to Dover, Delaware to present at and moderate a one-day conference on the health care challenges of reaching vulnerable immigrant worker populations.
About 30 clinicians from Delaware community health centers and community organizations attended the conference, co-sponsored by MCN, Johns Hopkins Education and Research Center for Occupational Safety and Health (Johns Hopkins ERC), and the New York Center of Agricultural Medicine and Health (NYCAMH). Liebman’s presentation was followed by a second presentation session offered by Rosemary Sokas, MD, MOH, Professor at Georgetown University, Health Professions School and MCN Board Member, and John May, MD, MPH, of Bassett Healthcare Network. The participants then headed into a panel discussion on health care services, and a second panel on advocacy groups, before closing the jam-packed conference in the late afternoon.
The organizers dove into a vast array of concerns for immigrant worker populations, from occupational health concerns like pesticide exposure, construction hazards, and silica cement, to access issues for undocumented workers, to the nature of change in immigration, in Delaware and around the world.
Here are the top five take-away messages from the one-day conference:
- We are a nation of immigrants. But today’s migration patterns don’t resemble what we saw 40 years ago, Liebman said during her presentation, which kicked off the conference. Our global world economy, improved communication, ease of transportation combined with increasing social inequalities have accelerated the pace of migration worldwide. Today, there are 244,000,000 living outside their home. If they were the population for a country, they’d be the fifth largest in the world. For health centers serving underserved populations, such a rapidly shifting immigration picture can drastically change what the immigrant worker community needs. Similarly, the changing political picture here in the US has already began to affect immigrant communities, with anecdotal evidence of an increase in no-show rates and a drop in appointments, as immigrants choose to avoid public spaces over fear of exposure. When Liebman asked the audience what changes, if any, they had experienced, one participant acknowledged this his health center had seen a 30 percent increase in no-show rates in recent months. Health center services need to be sufficiently nimble to respond to such newly arising barriers to care.
- Understand there are important “push” factors from sending countries and “pull” factors from receiving countries that foster immigration
- Be aware that workers and their families have limited access to legal entry into the US, although the number of temporary visas provided by the US are increasing.
- Recognize the risks patients take simply to work in the US.
- Make sure to enroll patients who are on the move or may be migrating in Health Network, MCN’s bridge case management system that is free for the enrolling clinic and the patient. Learn more at MCN’s Health Network page.
- Enabling services can’t be siloed. Liebman presented two case studies where patients’ serious occupational exposures weren’t connected to their health problems -- until outreach workers and interpreters, important members of the clinical team, connected the dots. In the famous case of Carlitos, a child born without legs or arms, it was an outreach worker serving the camps who uncovered a string of extremely uncommon birth defects in Florida, a pattern that wasn’t identified by a birth defects registry, or local physicians who delivered the babies. (The parents of Carlitos eventually settled their lawsuit against their employer, Ag-Mart.) Similarly, among multiple cases of a strange new neurological disease, Progressive Inflammatory Neuropathy, among pork processing workers, it was an interpreter who noticed that three patients for whom she interpreted had similar serious health issues, and alerted a clinician. Liebman’s point: the role of the clinical team as a whole can’t be overstated. Integrating services into the care approach is essential for immigrant workers whose occupational risks are complicated and varied. An integrated approach with a functioning care team brings better health results to the patients.
- Learn about developing a Patient Centered Medical Home for workers on the move.
- Consider the entire household. Mixed-status households -- in which, for example, US citizen children live with their mother who lacks authorization to live and work in the US -- present a unique and oft-overlooked challenge for clinicians. The mental health effects of deportation on the children of the deported can be sudden and serious, and can be overlooked when the children are indeed not immigrants themselves. A US citizen child’s family may avoid health services for the child because of fear of exposure of the whole family. Clinicians are encouraged to ask about the whole family’s needs to get a fuller picture of life at home. CHWs in particular should be aware of the health needs of mixed-status households.
- Read some of the work Luis Zayas, Dean of the School of Social Work at the University of Texas at Austin and a member of MCN’s External Advisory Board, who has spent a decades researching the effects of deportation on US citizen children. Here’s one recent article from 2016, “Disrupting young lives: How detention and deportation affect US-born children of immigrants.”
- Read some of the work Luis Zayas, Dean of the School of Social Work at the University of Texas at Austin and a member of MCN’s External Advisory Board, who has spent a decades researching the effects of deportation on US citizen children. Here’s one recent article from 2016, “Disrupting young lives: How detention and deportation affect US-born children of immigrants.”
- The occupation of your patient is a key social determinant of health. Understanding the work your patient does is critical to providing quality care. For instance, an agricultural worker is more likely to be exposed to pesticides in the course of their work than workers in other industries. Being cognizant of the signs and symptoms of pesticide poisoning as well as strategies to help your patient prevent exposures is important.
- EPA’s Recognition and Management of Pesticide Poisonings Manual, 6th Edition: This manual is the seminal work for any clinician working with patients who may experience pesticide poisonings. Download your copy for free, or request a hardcopy on the EPA’s website.
- Environmental and Occupational Health Screening Questions for Primary Care: Make sure you’re asking the right questions with this list, in English and Spanish.
- Work on gaining trust. Toward the end of the conference, Charita Olabiyi, Director of the Farmworker Health Program and Outreach Manager for Westside Family Healthcare in Delaware, touched on a critical factor for reaching immigrant worker populations: trust. Gaining the trust of the community can be the key to providing effective health care. When a CHW is trusted, she will learn more about the specific health challenges of the community, how the culture of the community may cause different interactions with the health system, and more.
- Looking to expand your outreach team’s knowledge base on clinical concerns among immigrant workers? Our highly rated webinar series for CHWs in English and Spanish is archived on our website. Scroll down to see 2017’s series, which features information on five important clinical indicators: 1) Diabetes, 2) Prenatal Control, 3) Oral Health, 4) Hypertension, and 5) Mental health for health centers financed by HRSA.
- Keep tabs on our Upcoming Webinars page for regular webinars aimed at disseminating new models and best practices to health care providers serving immigrant workers.
How do you reach your immigrant worker populations? Let us know via email (chutkins-seda@migrantclinician.org) or on Facebook.
Like what you see? Amplify our collective voice with a contribution.
Got some good news to share? Send it to us via email, on Facebook, or on Twitter.
Return to the main blog page or sign up for blog updates here.